JULY 27, 2020
Initial Experience with a Minimally Invasive Sacroiliac Fusion Device, a Retrospective Case Series
David Kim, MD1; Dawood Sayed1; Christopher Lam1, Brian Kim1, Angelica Ortiz2, Stephen Pyles2
1Department of Anesthesiology, University of Kansas Medical Center, Kansas City, Kansas
2Pain Treatment Centers, Ocala, Florida

Background
- Sacroiliac joint mediated pain is a common yet under-recognized source of chronic pain accounting for up to thirty percent of lower back pain complaints in the general population.
- Sacroiliac fusion via a minimally invasive, posterior, percutaneous approach is a novel technique that is both safe and highly effective for treatment of sacroiliac joint dysfunction.
Purpose
- Purpose of this study was to investigate the safety and efficacy of a novel approach for SI joint fusion.
Hypothesis
- The hypothesis of this study is that with proper patient selection, minimally invasive sacroiliac joint fusion is a safe and effective tool for an underdiagnosed cause of refractory lower back pain.
Methods
- Sixteen patients with presenting with chief complaint of refractory lower back region pain and history, physical exam, and imaging findings consistent with SI joint pathology underwent diagnostic SI joint injections.
- Following response to diagnostic SI joint injections, SI joint fusion was performed via a minimally invasive, posterior, percutaneous approach.
- The system utilized was the “LinQ” SI joint fusion system (PainTEQ, Tampa, FL, USA).
- Opioid medication usage, numeric pain rating scale from 0 to 10, and percentage improvement were documented prior to fusion and at latest follow up interval.
- As the study is devoid of patient identifiable information, it is exempt from IRB review requirements as per Kansas University Medical Center policy.
Figures
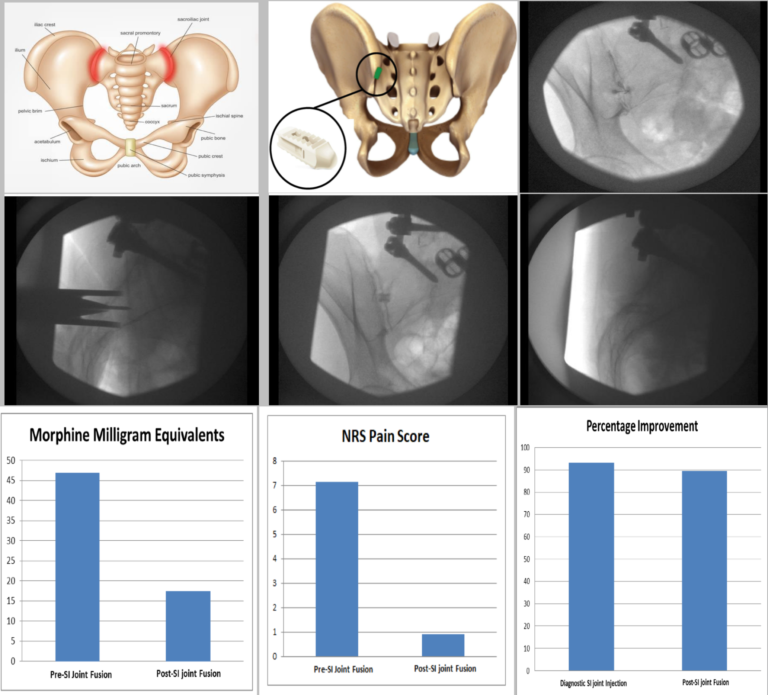
Figure descriptions:
Figure 1) Illustration of Sacroiliac Joint Inflammation and Pain. Figure 2) Illustration of minimally invasive posterior SI joint fusion device. Figure 3) Diagnostic SI joint injection.
Figure 4) Sagittal view of placement trocar. Figure 5) AP view of implant. Figure 6) Sagittal view of implant.
Figure 7) MME reduction with SI joint fusion. Figure 8) NRS Pain Score Reduction with SI joint Fusion. Figure 9) Sustained percentage improvement between diagnostic injection and SI joint fusion.
Results
- The average age of this patient group was 72.6 years.
- Gender was 50% (8/16) female.
- Of this population, 68.7% (11/16) patients had a spinal cord stimulator with successful ongoing treatment of a different lower back or lower extremity complaint.
- The average duration of SCS usage prior to SI fusion was 29.1 months.
- The average length of follow up after SI fusion was 6.3 months.
- Prior to fusion, average MME for patients taking opioids was 46.9.
- At latest follow up, average MME for these patients was 17.5.
- Average pre-fusion NRS was 7.15 ± 1.76, (95% CI 6.38 to 7.92).
- Average post-fusion NRS at latest follow up was 0.90 ± 1.97 (95% CI 0.04 to 1.76). This resulted in a mean decrease of 5.9 in NRS with paired t-value of -11.3243 (p < 0.00001).
- Average percentage improvement following diagnostic injection was 93.25% (95% CI 88.4% to 98.1%) and following fusion was 89.50% (95% CI 78.8% to 100%). No adverse events were observed.
Discussion
- This case series suggests that scroiliac joint mediated pain is a significant and under-recognized 1 source of chronic pain that can be refractory to neuromodulation.
- Sacroiliac joint mediated pain can be safely and effectively treated with a minimally invasive, posterior, percutaneous approach for SI fusion.
- Opioid consumption and NRS pain scores were significantly improved with sustained and significant global improvement after SI joint fusion via this technique.
References
1. Bernard TN, Kirkaldy-Willis WH. Recognizing specific characteristics of nonspecific low back pain. Clin Orthop. 1987;217:266-280.