Clinical Evidence and Research Support LinQ Posterior SI Joint Fusion as:
Simple
A single allograft implant, small incision, and streamlined 4-step procedure leads to reduced procedure time and hospital stay.
Safe
A posterior approach away from major nerves and arteries, and monitored sedation support fewer complications.
Effective
The pain and function improvement for LinQ treatment is similar when compared to major studies with lateral triangular SI rods.
Our commitment to clinical excellence through evidence generation.
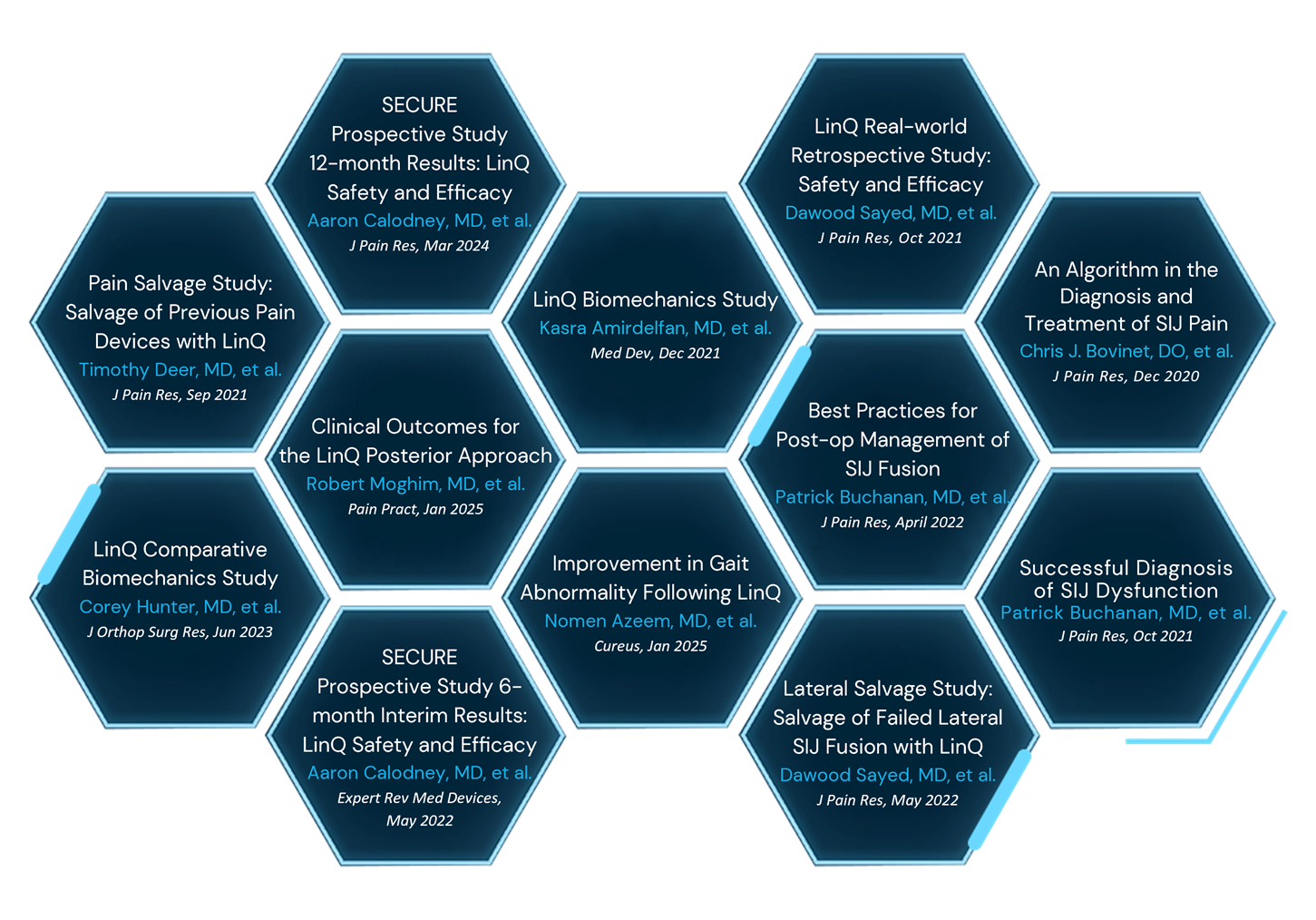
SECURE Prospective Study
12-month results
- LinQ showed similar improvement in pain and function at 12 months as the iFuse device as demonstrated in their studies
- VAS Pain Scores: 43.3 mean reduction at 12 months (from 76.2 mean to 32.6 mean) with 73.5% having ≥ 20 improvement
- ODI Function Scores: 25.3 mean improvement at 12 months (from 52.4 mean to 26.9 mean) with 68.7% having ≥ 15 improvement
Pain Salvage Study
Salvage of Previous Pain Devices with LinQ
LinQ demonstrated the potential to rescue patients who have had inadequate pain relief from previous therapies, including:
- Spinal cord stimulation
- Interspinous spacer
- Intrathecal drug delivery
- Minimally invasive lumbar decompression
Average Patient-reported Pain Relief:
67.6%
Average Pain Relief in Failed Back Surgery Syndrome Patients:
76.5%
Additional Supporting Evidence
LinQ Studies
Posterior Allograft Sacroiliac Joint Fusion with Pre-operative Mapping
A single-center, retrospective study of 208 patients receiving the LinQ procedure with pre-operative mapping of patient anatomy. The study demonstrated a significant mean pain improvement of 84% and a decrease of opioid consumption of 51.8% at the mean final follow-up of 18 months.
Improvement in Gait Abnormality Following Minimally Invasive Posterior Sacroiliac Joint Fusion
A single-arm, prospective, pilot study assessing gait characteristics on 10 patients who underwent the LinQ procedure by PainTEQ. Results demonstrated that average gait velocity improved significantly by 55.4% at 6 months. Gait speed, gait variability, and gait symmetry showed improvement, accompanied by a significant decrease in fall risk. This study marks a groundbreaking, first-ever objective evaluation of gait in patients who have undergone minimally invasive posterior SI joint fusion.
Clinical Outcomes for Minimally Invasive Sacroiliac Joint Fusion with Allograft using a Posterior Approach
An independent investigator-initiated retrospective analysis of 43 patients receiving the LinQ procedure. Results identified a mean VAS score reduction from 8.26 at baseline to 2.71 (67%) at 12 months and a statistically significant reduction in medication usage. No adverse events occurred.
SECURE Prospective Study 6-month Interim Results: LinQ Safety and Efficacy
At 6 months, a mean improvement of 34.9 was identified by a reduction in VAS and functional improvement was demonstrated by a mean reduction in ODI of 17.7. The posterior single-point transfixation is safe and efficacious for the treatment of sacroiliac joint dysfunction with statistical improvements in pain and function.
Lateral Salvage Study: Salvage of Failed Lateral SIJ Devices with LinQ
The study includes a total of 7 patients who underwent LinQ posterior SIJ fusion who had previously undergone lateral SIJ fusion. Results showed significant reductions in pain scores and opioid consumption, which suggests that the LinQ procedure may be a viable treatment option to salvage pain relief in those with failed lateral SIJ fusion devices. The mean patient-reported pain improvement following posterior fusion was 80%, with an average follow-up time of 10 months. Median morphine milliequivalents were 20 pre-procedure and 0 post-procedure.
LinQ Biomechanics Study
The LinQ procedure by PainTEQ provides a multifaceted mechanism for stabilizing the SI joint. First, by the reduction of the total range of motion in all planes of motion; second, by shifting the centers of the instantaneous axis of rotation towards the implant’s location in the predominant plane of motion. This combination minimizes movement at the implantation site, fostering osteointegration and fusion in the area.
Post-operative Management
Best Practices for Post-op Management of SIJ Fusion
SIJ fusion is a rapidly growing and evolving therapy with developing evidence to support its safety and efficacy. In the setting of a desired surgical outcome, safety and efficacy can be adversely impacted by poor post-operative care. The American Society of Pain and Neuroscience has created this best practice document in an effort to improve and standardize care in this critical time of patient recovery.
Diagnosis
Successful Diagnosis of SIJ Dysfunction
The diagnosis of SIJ pain is a multifaceted process that involves a careful assessment, including differentiating other pain generators in the region. This involves careful history-taking, appropriate physical examination, including provocative maneuvers, and diagnostic injections. Once the diagnosis is confirmed, long-term solutions may be considered, including recent advances in sacral lateral branch denervation and sacroiliac joint fusion.
A Review and Algorithm in the Diagnosis and Treatment of SIJ Pain
By synthesizing existing literature, the article provides a clearer algorithm that facilitates accurate diagnosis and effective management of SIJ dysfunction, improving patient care and outcomes. While conservative measures remain first-line treatments, interventional techniques and minimally invasive surgical options are viable for patients with persistent symptoms.
Reviews
American Society of Pain and Neuroscience Best Practice (ASPN) Guideline for the Treatment of Sacroiliac Disorders
While the quantity of evidence is currently more robust with the lateral approach given its preexistence, available studies suggest that that the posterior approach has at least similar efficacy with a lower risk profile
Review of Current Evidence for Minimally Invasive Posterior Sacroiliac Joint Fusion
While the lateral or transiliac approach has been well published, the posterior and posterior oblique approach has been recently introduced as an alternative means of stabilization of the SIJ. Preliminary case series presented reveal consistent decreases in pain scores and low complication rates.